course details
This Keratolytic Skin Disorders course is designed for Corneotherapists, Skin Treatment Therapists, Medical Aestheticians and Nurses, and provides a learning outcome of increased Knowledge for Clinical Referral and Intervention.
This master class covers the different keratolytic skin disorders commonly seen by today’s Skin diagnostician, Skin treatment therapist or Corneotherapist.
This class is a natural extension of education in the world of skin treatment therapy; the knowledge gained gives the confidence to “recognize, educate and refer” clients and patients.
The learning outcome of this course is a detailed understanding of common Keratolytic Skin Disorders, how to recognise them, when to refer on for specialist help or to plan in-clinic interventions.
A key outcome is for the practitioner to be able to speak knowledgably with clients or patients regarding common skin disorders so as to refer them on for further diagnosis if required.
Other learning outcomes of this course include:
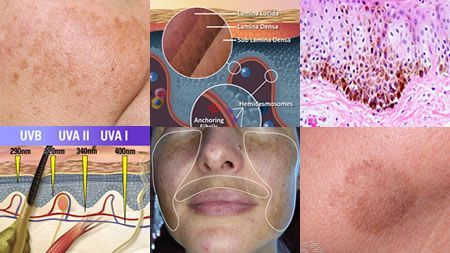
- How to recognize the difference between Skin Type and Risk Factors.
- How to recognize the difference between Skin Conditions, Skin Disorders, and Skin Disease.
- Understanding the relationship between intrinsic skin types and predispositions to disorders.
- Understand how specific disorders/diseases are categorised under the Texture/Colour/Secretions classifications.
- Understand the influences upon cells that lead to abnormal functioning that leads to skin disorders.
- Understand how the immune system can be the cause of skin conditions.
- Understand the different types of skin cancers and how to recognise them.
- Understand the pathology of inflammatory skin disorders such as Psoriasis.
- Understand the pathology of skin disorders of the pilosebaceous duct.
- Understand the pathology of benign epithelial lesions & tumours.
- Understand the pathology of Millia
- Understand the pathology of Dermatic and Seborrhoeic conditions.
- Understand the pathology of accumulative oxidised lesions such as Xanthelasma.
- Understand the pathology of eccrine related skin disorders.
- Understand the pathology of miscellaneous and other less common lesions and tumours affecting the hair follicle and sebaceous gland.
Prerequisites and prior learning:This course is designed for graduates of the Advanced Skin Analysis program, and refers back to prior learning from within the program.
Typical completion time (Including assessment) 4 hours, 50 minutes.Awarded 5 CPD points or 6.7 CE’s