I have often said that many of the modern skin conditions/disorders of today are caused by over treatment and/or over cleansing by the patient. This cleansing habit combined with the poor quality emulsifiers that are used in some cosmetics and the daily application of antibacterial substances has led to situations where the adaptive immune system begins to fail.
In addition to this “over cleansing” phenomenon is the lack of childhood exposure to infectious agents and microorganisms that also decreases an individuals susceptibility to disease. Cellular memory is not acquired and as a result many children have poor adaptive and innate immune systems because the over protective parent not only washes them too frequently, but does not allow them contact with the outside world and all the dirt and bacteria that go along with it.
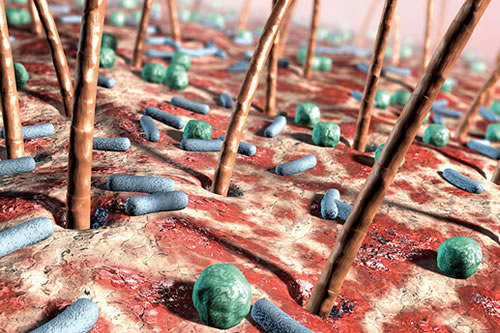
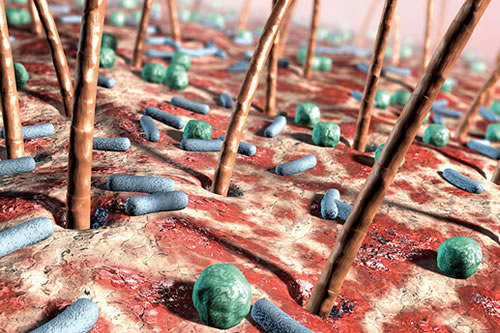
To take you back to the beginning; one must first remember the amount of natural flora (bacteria) that reside on the skin surface and that every healthy person has millions of bacteria living on the skin surface. It is on the mucous membranes of his / her nose, mouth etc and they all work in synergy to create the first line of skin barrier defence. We spread these bacteria from the mouth and nose on small, relatively heavy droplets of saliva and nose secret and shed skin scales during moderate physical activity, every person sheds approximately 1000 bacteria carrying skin scales per minute!
On the facial skin scales are bacteria such as Staphylococcus, Corneo-bacterium and Propionibacterium. These bacteria adhere to the skin scales and stay attached, even after shedding.
Contamination issues
The most important contamination of our environment is by these bacteria that travel on small skin scales (the mean size is 12 microns = thousandths of millimeter). They can be in the air of the skin treatment therapy room and sediment as an invisible dust on all surfaces as long as people in that room are shedding skin.
When the bacteria fall into suitable environment, such as an open wound, the bacteria begin to multiply. These bacteria do not cause any problems to us in our everyday lives, but when the first three lines of skin barrier defence are compromised, these bacteria can cause problems in the form of simple to very severe infections. But this isn’t the whole story, you will remember my writing about Dr Gallo and his early research into the Rosacea skin condition, and how it was established that an over-active innate immune system was an aggravating factor with this debilitating skin disorder.
The Anti-inflammatory Action of the Staphylococcal Bacteria
Dr Gallo and his fellow researcher Yi Ping Lai and colleagues have found many more new and wonderful things about the inflammatory response and wound healing skin since then.
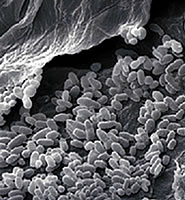
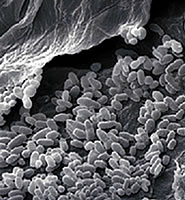
This newer information is linked to staphylococcal bacterial species that is present in the skin’s normal flora. (Discussed in first paragraph) In a healthy skin this bacterium resides on the skin surface without initiating inflammation, it is not until it becomes introduced below the stratum corneum that the bacteria induces an inflammatory response.
The researchers illustrated that bacteria on the skin surface triggers a pathway that prevents excessive inflammation after injury, which has uncovered elements of the wound repair response.(published Nature Medicine 2009-12-11)
In this groundbreaking study, Lai, Gallo and colleagues found a previously unknown mechanism by which a product of staphylococci inhibits skin inflammation. This inhibition is mediated by a molecule called staphylococcal lipo-teichoic acid (LTA), which acts on keratinocytes, in addition it was found that a Toll-like receptor 3 (TLR3) activation is required for normal inflammation after skin injury. “Keratinocytes require TLR3 to mount a normal inflammatory response to injury, and this response is kept from becoming too aggressive by staphylococcal LTA,” said Gallo.
In summary Dr Richard L. Gallo, MD, PhD, said in a press release: “To our knowledge these findings show for the first time that the skin epithelium requires TLR3 for normal inflammation after wounding and that the microflora helps to modulate this response.”
The researchers also found that Toll-like receptor 3 (TLR3) activation is required for normal inflammation after skin injury. This information is leading researchers to devise new therapeutic approaches for inflammatory skin disorders and related daily care. FBH
Further recommended reading: Surface bacteria maintain skin’s healthy balance
Further recommended reading: Understanding the skins microbiome